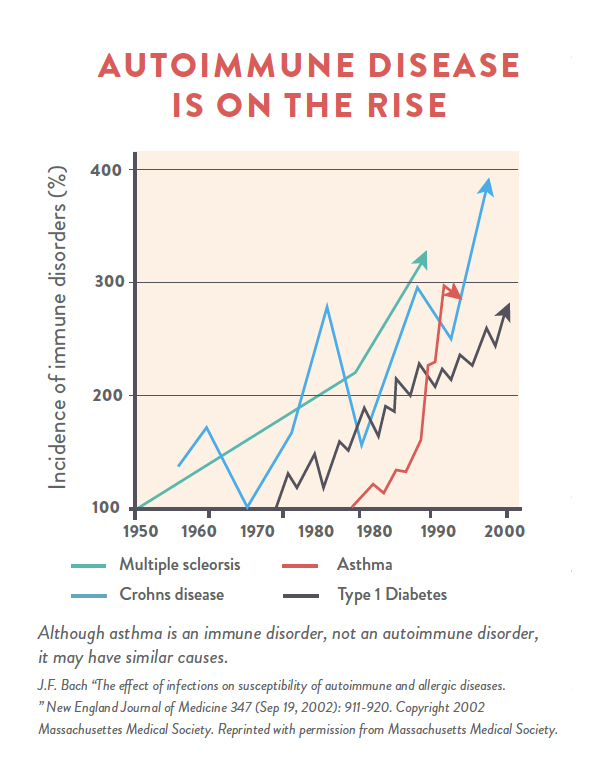
Autoimmune disease is an epidemic in our society, affecting an estimated 50 million Americans. But it doesn’t have to be. Although genetic predisposition accounts for approximately one-third of your risk of developing an autoimmune disease, the other two-thirds comes from your environment, your diet, and your lifestyle. In fact, experts are increasingly recognizing that certain dietary factors are key contributors to autoimmune disease, placing these autoimmune conditions in the same class of diet- and lifestyle-related diseases as type 2 diabetes, cardiovascular disease, and obesity. This means that autoimmune disease is directly linked to our food choices and how we decide to live your life. It also means that we can manage and reverse autoimmune disease simply by changing how you eat and making more informed choices about sleep, activity, and stress… and that’s some pretty darned good news!
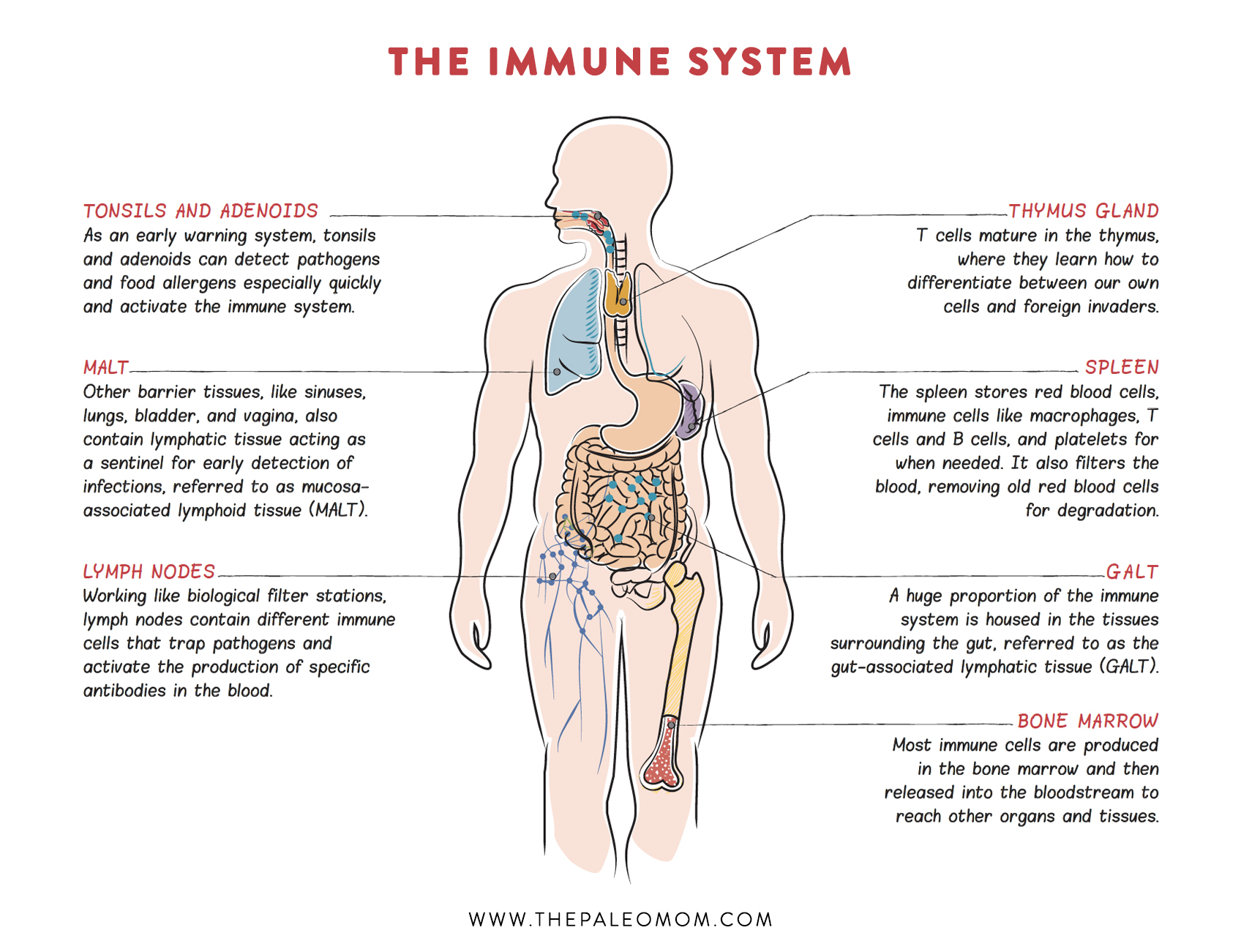
There are more than one hundred confirmed autoimmune diseases and many more diseases that are suspected of having autoimmune origins (download a complete list here). The root cause of all autoimmune diseases is the same: our immune system, which is supposed to protect us from invading microorganisms, turns against us and attacks our proteins, cells, and tissues instead. Which proteins, cells, and tissues are attacked determines the autoimmune disease and its symptoms. In Hashimoto’s thyroiditis, the thyroid gland is attacked. In rheumatoid arthritis, the tissues of your joints are attacked. In psoriasis, proteins within the layers of cells that make up your skin are attacked.
How does the immune system get so confused that it starts to attack our own bodies? It turns out that autoimmunity, the ability for the immune system to attack native tissues, is a relatively common accident. In fact, about 30% of people will have measurable levels of autoantibodies (antibodies that bind to some protein in our bodies instead of, or in addition to, a foreign protein, called an antigen) in their blood at any given time. In fact, this accident is so common, that our immune system has several failsafes for identifying autoimmunity and suppressing it. What occurs in autoimmune disease isn’t just the accident of autoimmunity, but also failure of the immune system failsafes, stimulation of the immune system to attack, and the build up of enough damage in cells or tissues within the body to manifest as symptoms of a disease.
This confluence of events that culminates in autoimmune disease is a result of the interactions between your genes and your environment—a perfect storm of factors that cause the immune system to be unable to distinguish self (you) from invader (not you).
The Paleo Autoimmune Protocol, typically abbreviated AIP, is a powerful strategy that uses diet and lifestyle to regulate the immune system, putting an end to these attacks and giving the body the opportunity to heal.
What is the AIP?
The Autoimmune Protocol, abbreviated AIP, is a complementary approach to chronic disease management focused on providing the body with the nutritional resources required for immune regulation, gut health, hormone regulation and tissue healing while removing inflammatory stimuli from both diet and lifestyle. The AIP diet provides balanced and complete nutrition while avoiding processed and refined foods and empty calories. The AIP lifestyle encourages sufficient sleep, stress management and activity as these are important immune modulators.
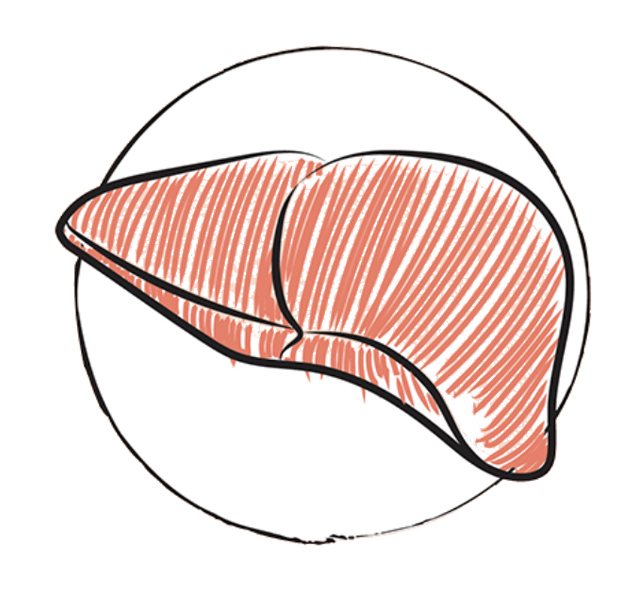
Foods can be viewed as having two kinds of constituents within them: those that promote health (like nutrients!) and those that undermine health (like inflammatory compounds). (While there are constituents that neither promote nor undermine health, they are not used to evaluate the merit of an individual food.) Some foods are obvious wins for a health-promoting diet because they have tons of beneficial constituents and very few or no constituents that undermine health—good examples of these superfoods are organ meats, seafood, and most vegetables. Other foods are obvious fails because they have a relative lack of health-promoting constituents and are rife with problematic compounds—good examples are gluten-containing grains, peanuts, and most soy products. But many foods fall into the amorphous world of gray in between these two extremes. Tomatoes, for example, have some exciting nutrients, but they also contain several compounds that are so effective at stimulating the immune system that they have been investigated for use in vaccines as adjuvants (the chemicals in vaccines that enhance your immune response to whatever you’re getting immunized against). The biggest difference between the Autoimmune Protocol and other dietary templates that take a nutrients-first approach while considering inflammation triggers is where we draw the line between “yes” foods and “no” foods in order to get more health-promoting compounds and fewer detrimental compounds in our diet. Those who are typically quite healthy can tolerate less-optimal foods than those who aren’t. You can think of the Autoimmune Protocol as a pickier version of other evidence-based dietary templates; it accepts only those foods that are clear winners.
As such, the Autoimmune Protocol places greater emphasis on the most nutrient-dense foods in our food supply, including organ meat, seafood, and vegetables. And the Autoimmune Protocol eliminates foods endorsed by other healthy diets that have compounds that may stimulate the immune system or harm the gut environment, including nightshades (like tomatoes and peppers), eggs, nuts, seeds, and alcohol. The goal of the Autoimmune Protocol is to flood the body with nutrients while simultaneously avoiding any food that might be contributing to disease (or at the very least interfering with our efforts to heal).
The AIP is an elimination diet strategy, cutting out the foods that are most likely to be holding back our health. After a period of time, many of the excluded foods, especially those that have nutritional merit despite also containing some (but not too much) potentially detrimental compounds, can be reintroduced. The AIP is not a life sentence, but rather a toolbox full of strategies for understanding how your body reacts to foods, lifestyle and your environment and methodologies for healing given your individual health challenges.
The AIP is also a holistic approach to health, including not only a dietary framework but also a focus on lifestyle factors known to be important modulators of immune function, gut health, and hormone health. This includes a strong focus on getting adequate sleep, managing stress, and living an active lifestyle while avoiding overtraining. These three lifestyle factors are each essential for gut health because they directly influence the gut microbiome (getting enough sleep, keeping stress levels in check, and being active are all essential for a healthy and diverse gut microbial community in addition to supporting the growth of key probiotic strains). Chronic stress and overtraining also increase intestinal permeability. Sleep, stress and activity are all essential hormone modulators; for example, insulin sensitivity is more strongly influenced by these lifestyle factors than it is by diet. And, most importantly, immune function is directly tied to lifestyle. Inflammation is triggered by getting inadequate less, feeling stressed, being sedentary, and overtraining. Furthermore, the regulatory aspects of the immune system are most active while we’re sleeping, and sleep quality is linked to stress. Additionally, there’s emerging evidence that a strong sense of connection and community as well as spending time in natural environments also contribute to a healthier immune system.
Drawing on insights gleaned from more than 1,200 scientific studies, the AIP is now supported by clinical trial evidence.
In a 2017 study, fifteen patients with active inflammatory bowel disease were placed on the Autoimmune Protocol by transitioning gradually over 6 weeks, followed by a 5-week maintenance phase. Patients were closely monitored and given access to health coaching. They were also given two books The Paleo Approach by Dr. Sarah Ballantyne, PhD (which remains the definitive AIP guidebook) and The Autoimmune Wellness Handbook by Mickey Trescott, NTP and Angie Alt, NTC, CHC, as resources for following the protocol. Clinical remission was achieved by week 6 (yes, just by completing the transition to the AIP) in eleven of the fifteen participants (73%!!), and they stayed in remission throughout the 5-week maintenance phase of the study. All patients, including those that didn’t achieve clinical remission, experienced quantifiable improvement in disease activity over the entire course of the study.
In a similarly-designed 2019 study, seventeen women with Hashimoto’s thyroiditis were placed on the Autoimmune Protocol by transitioning gradually over 6 weeks, followed by a 4-week maintenance phase. Patients experienced a statistically significant improvement in health-related quality of life scores as measured by the 36-Item Short Form Health Survey and Cleveland Clinic Center for Functional Medicine’s Medical Symptoms Questionnaire (MSQ). In fact, the clinical symptom burden, as measured by the MSQ, decreased from an average of 92 at the beginning of the study to 29 after the 10 weeks. This was accompanied by statistially significant reductions in C-reactive protein (a measurement of systemic inflammation) and white blood cell counts! See also Paleo Diet Clinical Trials and Studies.
The clinical research studies performed using the Wahls Protocol in multiple sclerosis provide additional validation for the Autoimmune Protocol. While there are a handful of foods included on the Wahls Protocol (most notably nightshades) that are excluded on the Autoimmune Protocol, the two protocols are remarkably similar despite the different philosophies that went into their formulation. The Wahls Protocol framework was developed with mitochondrial health as its primary goal whereas the Autoimmune Protocol framework was developed with immune regulation and gut health and its primary goals. It so happens that the nutrients required for mitochondrial health are nearly identical to those required for immune and gut health, hence the high degree of overlap between both approaches.
A growing number of clinicians, especially functional and integrative medicine specialists, are recommending the AIP to their patients, adding to the large body of anecdotal evidence supporting the efficacy of the Autoimmune Protocol. Most exciting, there is ongoing clinical research to quantify improvement in specific autoimmune diseases with a short-term intervention with the AIP, including research in Hashimoto’s thyroiditis. As the results from more and more clinical trials are published, there is increasing attention being paid to diet and lifestyle, not as a complementary approach to autoimmune disease management, but as a first-line course of treatment.
How Does The Autoimmune Protocol Work?
The Paleo Autoimmune Protocol works by addressing four key areas known to be important contributors to chronic and autoimmune diseases. Drawing on insights gleaned from more than 1,200 scientific studies, these diet and lifestyle recommendations specifically target:
 Nutrient density. The immune system (and indeed every system in the body) requires an array of vitamins, minerals, antioxidants, essential fatty acids, and amino acids to function normally. Micronutrient deficiencies and imbalances are key players in the development and progression of autoimmune disease. Focusing on consuming the most nutrient-dense foods available enables a synergistic surplus of micronutrients to correct both deficiencies and imbalances, thus supporting regulation of the immune system, hormone systems, detoxification systems, and neurotransmitter production. A nutrient-dense diet further provides the building blocks that the body needs to heal damaged tissues.
Nutrient density. The immune system (and indeed every system in the body) requires an array of vitamins, minerals, antioxidants, essential fatty acids, and amino acids to function normally. Micronutrient deficiencies and imbalances are key players in the development and progression of autoimmune disease. Focusing on consuming the most nutrient-dense foods available enables a synergistic surplus of micronutrients to correct both deficiencies and imbalances, thus supporting regulation of the immune system, hormone systems, detoxification systems, and neurotransmitter production. A nutrient-dense diet further provides the building blocks that the body needs to heal damaged tissues. Gut health. Gut dysbiosis and leaky gut are key facilitators in the development of autoimmune disease. The foods recommended on the Autoimmune Protocol support the growth of healthy levels and a healthy variety of gut microorganisms. Foods that irritate or damage the lining of the gut are avoided, while foods that help restore gut barrier function and promote healing are endorsed. Lifestyle factors that strongly influence gut barrier health as well as gut microbial composition are also addressed on the Autoimmune Protocol. Because of the link between gut health and immune function, restoring a healthy gut barrier and microbiome are necessary precursors to healing.
Gut health. Gut dysbiosis and leaky gut are key facilitators in the development of autoimmune disease. The foods recommended on the Autoimmune Protocol support the growth of healthy levels and a healthy variety of gut microorganisms. Foods that irritate or damage the lining of the gut are avoided, while foods that help restore gut barrier function and promote healing are endorsed. Lifestyle factors that strongly influence gut barrier health as well as gut microbial composition are also addressed on the Autoimmune Protocol. Because of the link between gut health and immune function, restoring a healthy gut barrier and microbiome are necessary precursors to healing. Hormone regulation. What we eat, when we eat, and how much we eat affect a variety of hormones that interact with the immune system. When dietary factors (like eating too much sugar or grazing rather than eating larger meals spaced farther apart) dysregulate these hormones, the immune system is directly affected (typically stimulated). The Paleo Autoimmune Protocol diet is designed to promote regulation of these hormones, thereby regulating the immune system by proxy. These and other essential hormones that impact the immune system are also profoundly affected by how much sleep we get, how much time we spend outside, how much and what kinds of activity we get, and how well we reduce and manage stress.
Hormone regulation. What we eat, when we eat, and how much we eat affect a variety of hormones that interact with the immune system. When dietary factors (like eating too much sugar or grazing rather than eating larger meals spaced farther apart) dysregulate these hormones, the immune system is directly affected (typically stimulated). The Paleo Autoimmune Protocol diet is designed to promote regulation of these hormones, thereby regulating the immune system by proxy. These and other essential hormones that impact the immune system are also profoundly affected by how much sleep we get, how much time we spend outside, how much and what kinds of activity we get, and how well we reduce and manage stress.
- Immune system regulation. Immune regulation is achieved by restoring a healthy diversity and healthy amounts of gut microorganisms, restoring the barrier function of the gut, providing sufficient amounts of the micronutrients required for the immune system to function normally, and regulating the key hormones that in turn regulate the immune system. The Autoimmune Protocol diet and lifestyle provide both the resources and the opportunity for immune regulation. Immune regulation combined with tissue healing account for reductions in symptoms.
Inflammation is a factor in all chronic illnesses, and this is one area where the foods we eat can make a huge difference. In some cases, an immune system that isn’t regulating itself properly directly causes the illness; in others, inflammation is merely an element of the illness or a contributor to how the illness came about—but it is always a player and a problem. What this means is that reducing inflammation and giving the immune system the resources it needs, as well as the opportunity to regulate itself, can help in every single chronic illness. This is important because inflammation is strongly influenced by what we eat, how well we sleep, how stressed we are, and how active we are. And this is why chronic illness can respond so positively to changes in diet and lifestyle.
Food has therapeutic potential for every chronic illness—but that’s not the same thing as calling food a cure. Depending on the illness you’re struggling with, how long you’ve had it, how aggressive the disease is, and what confounding factors you’re dealing with, dietary changes may get you as far as a complete reversal of your disease, or they may slow the progress of your illness, or they may simply improve your quality of life. These are all successes worth celebrating. Good food may not be the miracle cure you’re hoping for, but it’s pretty darn powerful all the same.
As you adopt the Paleo Autoimmune Protocol, your food choices become focused on consuming the nutrients to support this healing—foods that provide everything your body needs to stop attacking itself, repair damaged tissues, and get healthy again: proteins, carbohydrates, and fats to sustain a normal metabolism, build new tissue, and produce hormones, important proteins, and signaling molecules; and the full range of fat-soluble vitamins, water-soluble vitamins, minerals, and antioxidants to get rid of inflammation, regulate the immune system, and support the normal functioning of all the body’s systems.
Learn Everything You Need to Know about the AIP!
RETIREMENT SALE! SAVE 70% OFF!
I am loving this AIP course and all the information I am receiving. The amount of work you have put into this is amazing and greatly, GREATLY, appreciated. Thank you so much. Taking this course gives me the knowledge I need to understand why my body is doing what it is doing and reinforces my determination to continue along this dietary path to heal it. Invaluable!! –Carmen Maier
The AIP Lecture Series is your ultimate resource for the Autoimmune Protocol.
What To Eat and What To Avoid
Following the AIP diet involves increasing your intake of nutrient-dense, health-promoting foods while avoiding foods that may be triggers for your disease.
In summary, the rules of what to eat are:
- organ meat and offal (aim for 5 times per week, the more the better)–read more here.
- fish and shellfish (wild is best, but farmed is fine) (aim for at least 3 times per week, the more the better)–read more here and here.
- vegetables of all kinds, as much variety as possible and the whole rainbow, aim for 8+ servings daily
- Leafy green vegetables (lettuce, spinach, kale, collards, celery leaves, etc.)
- Colorful vegetables and fruit (red, purple, blue, yellow, orange, white)
- Cruciferous vegetables (broccoli, cabbage, kale, turnips, arugula, cauliflower, Brussels sprouts, watercress, mustard greens, etc.)
- Roots, tubers and winter quash (cassava, sweet potato, parsnip, beets, fennel, carrots, rutabaga, turnip, acorn squash, spaghetti squash, etc.)
- Onion family (aka alliums, onions, leek, garlic, ramps, etc.)
- Sea vegetables (excluding algae like chlorella and spirulina which are immune stimulators)
- Mushrooms (and other edible fungi)
- herbs and spices
- quality meats (grass-fed, pasture-raised, wild as much as possible) (poultry in moderation due to high omega-6 content unless you are eating a ton of fish)
- healthy fats (pasture-raised/grass-fed animal fats [rendered or as part of your meat], fatty fish, olive oil, avocado oil, coconut oil, palm oil[not palm kernel])
- fruit (keeping fructose intake between 10g and 40g daily-note that 20g is probably optimal)
- probiotic/fermented foods (fermented vegetables or fruit, kombucha, water kefir, coconut milk kefir, coconut milk yogurt, supplements)–read about them here and here.
- glycine-rich foods (anything with connective tissue, joints or skin, organ meat, and bone broth)
- gut microbiome superfoods ( high-fiber and phytonutrient fruits and vegetables, cruciferous vegetables, mushrooms, roots, tubers, alliums, leafy greens, berries, apple family, citrus, extra virgin olive oil, fish, shellfish, honey and bee products, fermented foods, edible insects, tea, and bone broth)
- Source the best-quality ingredients you can.
- Eat as much variety as possible
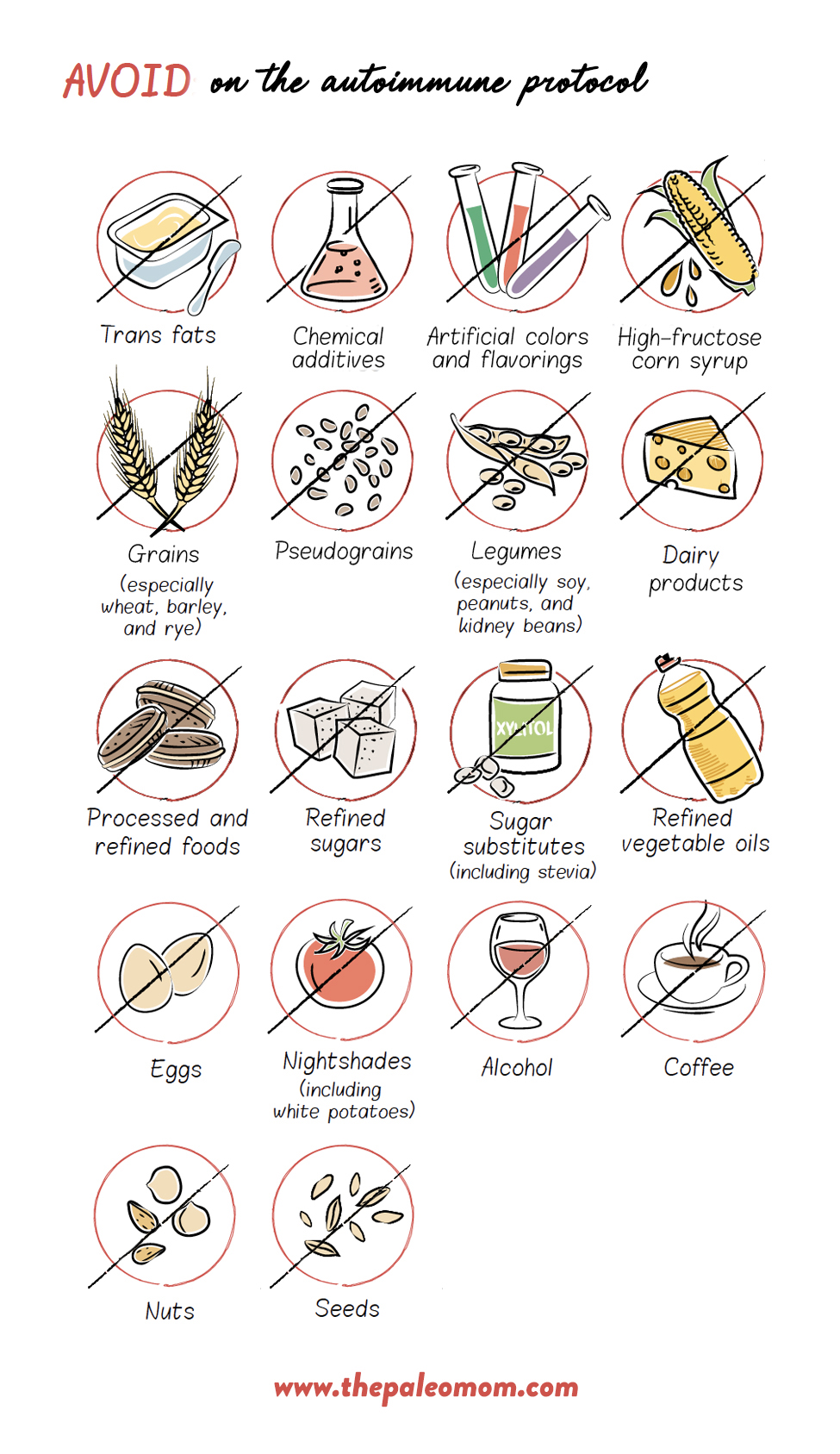
In addition, remove the following from your diet:
- Grains
- Legumes
- Dairy
- Refined and processed sugars and oils
- Eggs (especially the whites)
- Nuts (including nut butters, flours and oils)
- Seeds (including seed oil, cocoa, coffee and seed-based spices)
- Nightshades (potatoes [sweet potatoes are fine], tomatoes, eggplants, sweet and hot peppers, cayenne, red pepper, tomatillos, goji berries etc. and spices derived from peppers, including paprika)
- Potential Gluten Cross-Reactive Foods
- Alcohol
- NSAIDS (like aspirin or ibuprofen)
- Non-nutritive sweeteners (yes, all of them, even stevia and monk fruit)
- Emulsifiers, thickeners, and other food additives
Moderate your intake of the following:
- Fructose (from fruits and starchy vegetables, aiming for between 10g and 40g daily-note that 20g is probably optimal)
- Salt (using only unrefined salt such as Himalayan pink salt or Celtic gray salt)
- High-glycemic-load fruits and vegetables (such as dried fruit, plantain, and taro root) – note, the AIP is not low-carb (see The Case for More Carbs: Insulin’s Non-Metabolic Roles in the Human Body)
- Omega-6 polyunsaturated fatty acid–rich foods (such as poultry and fatty cuts of industrially produced meat)
- Black and green tea (up to 3-4 cups per day is okay for most people)
- Coconut
- Natural sugars (honey and blackstrap molasses are the best choice)
- Saturated fat (aiming for 10-15% of total calories)
This diet is appropriate for everyone with diagnosed autoimmune disorders or with suspected autoimmune diseases. It is very simply an extremely nutrient-dense diet that is devoid of foods that irritate the gut, cause gut dysbiosis and activate the immune system. You will not be missing out on any nutrients and this diet is absolutely appropriate to follow for the rest of your life. If you have a specific autoimmune disease that causes extra food sensitivities, those should be taken into account with your food choices.
Lifestyle Factors
Don’t forget the crucial importance of: getting enough sleep (at least 8-10 hours every night), managing stress (mindful meditation is very well studied in the scientific literature and universally shown to be beneficial), protecting circadian rhythms (being outside during the day, being in the dark at night and avoiding bright lights in the evening), enjoying nature, nurturing social connection, having fun, making time for hobbies, relaxing, and getting lots of mild to moderately intense activity (while avoiding intense/strenuous activity). Read more about the Paleo lifestyle here.
Elimination and Reintroduction
The autoimmune protocol can be thought of as a nutritional intervention for a diet gone badly awry, overabundant in calories and lacking in vital nutrients. But how well an individual tolerates suboptimal foods—whether we’re talking about something like tomatoes, which are included in the Paleo diet but eliminated on the autoimmune protocol, or something like grains, which are not included in either nutritional approach—depends on nutrient status, stress, sleep, activity level, genetics, and health history. As we improve these factors with diet and lifestyle changes, it’s fairly common to see tolerance of certain foods increase.
The autoimmune protocol is an elimination diet at its core (following AIP guidelines 100% is often termed the elimination phase), designed to cut out the most likely food culprits while flooding the body with nutrients. And the best part about an elimination diet is that, eventually, you get to reintroduce foods that you’ve been avoiding.
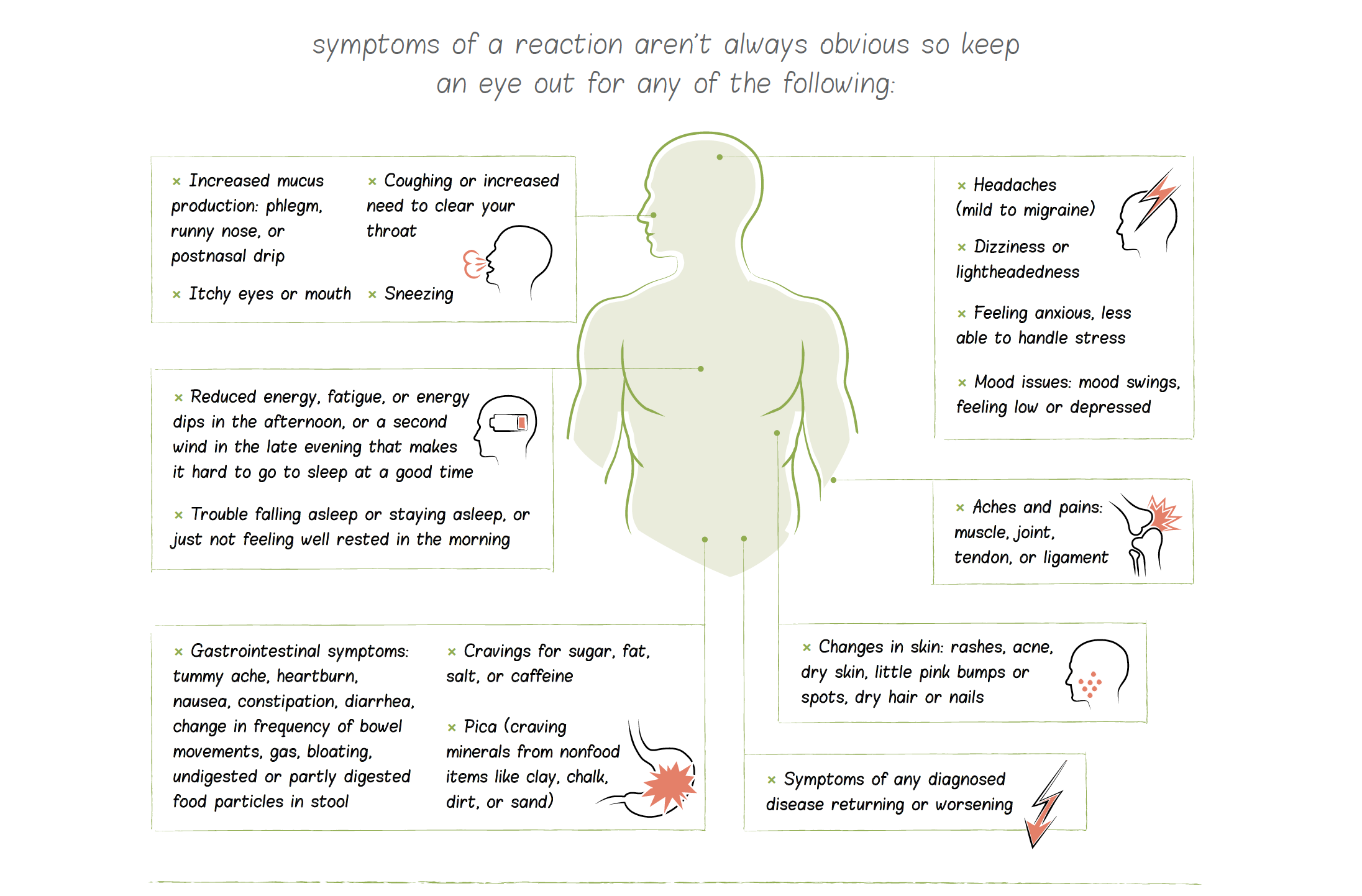
Read more about reintroductions, including how to go about it, when to do it, what to watch for, and which foods to tackle first, here.
It’s a surprisingly common experience to feel so good on the AIP that a person is afraid to try any reintroductions. But reintroducing eliminated foods is a critical step of your health journey. This is because some eliminated foods (like eggs, nuts, seeds, cocoa, and grass-fed dairy) have some impressive nutritive value and can improve the overall nutrient density of your diet if well tolerated. Plus, the more dietary flexibility you have, the easier life is—you’ll have less difficulty traveling or eating in restaurants or at potlucks, work meetings, or any social situation.
The knowledge you glean from reintroductions is empowering. If a reintroduction goes well, you’ve got anew food to add to your diet, increasing the variety of foods you eat. If a reintroduction doesn’t go well, this is still great information! You now better understand the dietary triggers of your disease and which lines you can’t cross. And in the uncommon case where a reintroduction goes very poorly (the fear of which is what stops many people from even trying), remember that the AIP is an entire toolkit for healing. You have the knowledge and skills to recover quickly and get back on your feet. Just go back to 100 percent AIP, get plenty of sleep and low-strain activity, and stay hydrated until you feel better.
Get the Definitive Resources for the Autoimmune Protocol
The Autoimmune Protocol Lecture Series is a 6-week video-based, self-directed online course that will teach you the scientific foundation for the diet and lifestyle tenets of the Autoimmune Protocol. Think of this course as going to college for your health! The AIP Lecture Series doesn’t shy away from teaching important scientific concepts. Dr. Sarah Ballantyne, PhD firmly believes that understanding how foods affect our health and the cellular level is an essential motivator for making positive and lasting change, as well as being critical to the self-discovery processes of finding individual tolerance and reintroduction. But, you don’t need a science background to take this course! Dr. Sarah explains the scientific evidence for each facet of the Autoimmune Protocol in her signature approachable style using accessible language and visual guides. If you enjoy Dr. Sarah’s books or articles on this website, you’ll love this course!
The Autoimmune Protocol E-Book is a comprehensive quick-start guide for everyone new to the AIP but it also serves the additional function of updating the Autoimmune Protocol to reflect new knowledge and provide a direct way to communicate with those in the AIP community regarding these (and possible future) tweaks. With this all-in-one e-book, you’ll be able to hone in on the new information that matters most, including 300+ pages of quick-access information on the AIP, new information on why nutrient sufficiency and gut health are a primary focus of the AIP, 4 weeks of meal plans with shopping lists, over 80 family-friendly recipes, and more!
The Paleo Approach is the New York Times bestselling complete guide to using diet and lifestyle to manage autoimmune disease and other chronic illnesses. With over 400 pages of scientific explanations of the why’s, what’s, and how’s behind diet and lifestyle recommendations to help regulate the immune system and provide the body with the opportunity to heal. This encyclopedic resource also contains tons of practical information including tips for transitions, working with your doctor, medical test and treatments that might be helpful, troubleshooting, and when and how to reintroduce foods. This book goes into scientific detail, while keeping explanations accessible and fun to read, and includes over 1200 scientific references. This is the book for people who want to understand the contemporary science behind how the food we eat as well as how we live our daily lives together impact our bodies to either promote health or facilitate disease.
The Paleo Approach Cookbook is the National bestselling companion cookbook to The Paleo Approach! The Paleo Approach Cookbook is over 400 pages and includes over 200 recipes, all strict autoimmune protocol (AIP), and lots of resources (over 100 pages worth!) to help you be successful in the kitchen while you tackle the diet recommendations in The Paleo Approach. With such a huge number of recipes (that each include cook time, prep time, servings, tips, variations, nutrition facts, FODMAP alerts), as well as hundreds of recipe variations, there’s something for everyone! The Paleo Approach Cookbook also includes a summary of the diet, cooking guides, kitchen How-Tos, shopping lists, food storage guides, kitchen tool essentials, cooking glossary of terms, time management strategies, how to read labels, recipe Top Ten, alphabetical Yes-No-Maybe-So list of foods, 6 one-week meal plans (two of which are low-FODMAP) and MORE!
Achieving health through nutritious food choices has never been simpler nor more delicious thanks to The Healing Kitchen! This cookbook makes healing using the Autoimmune Protocol completely accessible to everyone, regardless of your budget, time limitations, or access to specialty grocers. Armed with more than 175 budget-friendly, quick and easy recipes made with everyday ingredients, you get to minimize time and effort preparing healthful foods without sacrificing flavor! Straightforward explanations and a comprehensive collection of visual guides will teach you which foods are the best choices to mitigate chronic illnesses, including autoimmune disease. Real-life practical tips on everything from cleaning out your pantry and easy ingredient swaps to reinventing leftovers and DIY flavor combinations will help you go from theory to practice effortlessly. Even better, twelve 1-week meal plans with shopping lists takes all the guesswork out of your weekly trip to the grocery store!
For more recommendations on books, programs, and blogs to follow, check out my AIP Community page!
Need More Guidance?
An AIP Certified Coach is a practitioner who has received advanced training in addition to their base certification on the science behind autoimmune diseases and the AIP as well as practical strategies for helping clients implement dietary and lifestyle interventions to best affect healing and achieve higher levels of wellness.
These health and wellness practitioners from across the globe each have their own stories of illness, struggle and healing, their own inspirational context that led to their commitment to serve the autoimmune community. Their overarching philosophy is that real health begins with eating REAL food and adopting a lifestyle that is conducive to long-term health. At the same time, AIP Coaches recognize the individual nature of each person’s body and the many paths to wellness. They are here to meet you where you are and be your dedicated support in finding the correct approach for you.
AIP Coaches can provide you with personalized support for all stages of your journey on the Autoimmune Protocol. Working one-on-one with an AIP Certified Coach, you’ll be able to clarify when you’re moving in the right direction and receive guidance when you’re off course.
AIP Coaches work with the unique individuality of each client by using assessment tools like questionnaires and food journals. They make personalized plans for each client based on their distinct needs—no one-size-fits-all approach! Their method is flexible and adaptable to a wide variety of goals and situations.
If you are transitioning to the AIP, your AIP Coach can provide you with information, motivation and accountability, supporting your customized transition plan with tangible resources such as meal plans, shopping lists, lifestyle guides, and practical strategies for fitting the AIP into your life. Once you have fully adopted the AIP, your AIP coach can providing you with emotional support for sustaining this protocol throughout the healing process. Not seeing the results you expected or dealing with additional health challenges? Your AIP Coach can help you troubleshoot and refine your implementation so that you get the most out of the AIP. Your AIP Coach can also guide you through the reintroduction phase, creating an individualized plan for reintroduction priorities, helping you to identify subtle indicators of reactions, and providing advice on handling unexpected severe food reactions. Have you been riding the AIP rollercoaster? Your AIP Coach can help you identify and find solutions to your own personal challenges to implementation and maintenance of the protocol. Just need your own personal cheerleader? Yep, your AIP Coach can do that too.

Often, healing just means putting the right practices in place. Your AIP Coach is your expert guide for doing so in a customized way. They want to help you discover the true foundations of good health and support you every step of the way! Your body can heal itself—it just needs the right tools!
Each AIP Coach focuses their practice slightly differently, and no matter what your health and wellness needs, you’ll find support that’s right for you. Find an AIP Coach near you, or one who works with clients long-distant, in the AIP Certified Coach Directory: http://aipcertified.com/coach-directory/
If you are a healthcare professional interested in this high-value certification, join my Healthcare Professionals e-mail list by clicking here (make sure to select the Healthcare Professional list and any other lists you’re interested in!). I will e-mail you with more information on how to become an AIP Certified Coach.
Learn Everything You Need to Know about the AIP!
RETIREMENT SALE! SAVE 70% OFF!
I am loving this AIP course and all the information I am receiving. The amount of work you have put into this is amazing and greatly, GREATLY, appreciated. Thank you so much. Taking this course gives me the knowledge I need to understand why my body is doing what it is doing and reinforces my determination to continue along this dietary path to heal it. Invaluable!! –Carmen Maier
The AIP Lecture Series is your ultimate resource for the Autoimmune Protocol.